Turbinate reduction surgery is a medical procedure that addresses nasal obstruction and improves breathing by reducing the size of nasal turbinates. While the surgery can offer relief for individuals suffering from nasal congestion and related issues, the question of insurance coverage often arises.
In this comprehensive blog post, we will explore the factors that influence insurance coverage for turbinate reduction surgery, the medical necessity criteria, and tips for navigating the insurance process.
What Are Nasal Turbinates?
Nasal turbinates are structures inside the nasal passages responsible for humidifying and filtering air. However, they can become swollen and inflamed due to various factors, leading to nasal congestion, difficulty breathing, and other related problems. Comprising three pairs—superior, middle, and inferior—these thin, bony structures are covered by a mucous membrane.
Despite their essential role in maintaining optimal respiratory conditions, enlarged turbinates can cause nasal congestion, breathing difficulties, and other related issues. Understanding the anatomy and function of nasal turbinates is essential for addressing respiratory issues and exploring potential interventions like turbinate reduction surgery to restore normal nasal function.
Types of Turbinate Reduction Surgery
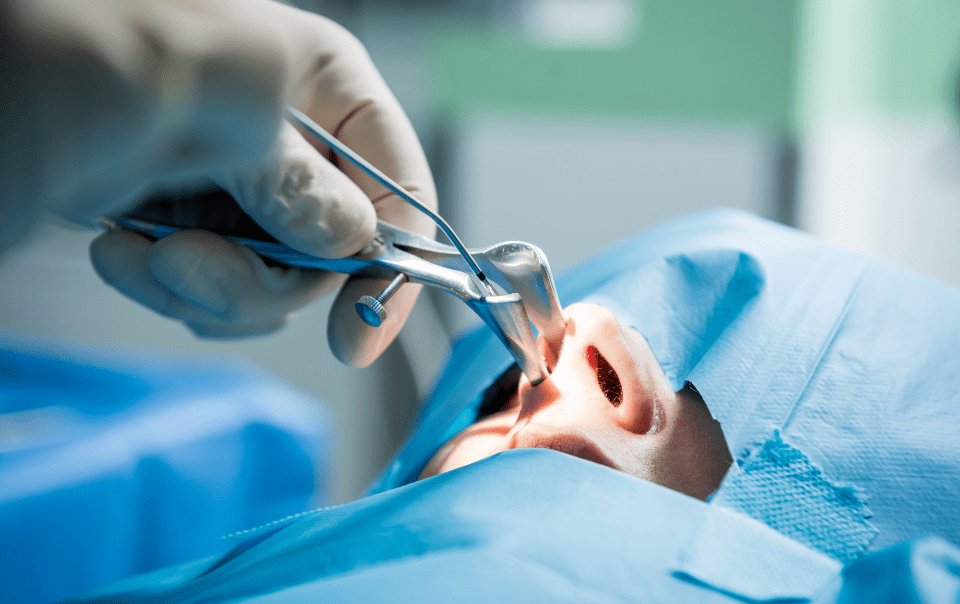
Turbinate reduction surgeries alleviate nasal obstruction and breathing difficulties caused by enlarged nasal turbinates. There are several types of turbinate reduction surgeries, each employing different techniques to achieve the desired outcome.
Radiofrequency Turbinate Reduction (RFTR) – In this minimally invasive procedure, radiofrequency energy is applied to the turbinates. The energy generates controlled heat to contract and shrink the enlarged tissues. RFTR is often performed in an outpatient setting.
Laser Turbinate Reduction – Laser energy is used to vaporize or shrink the excess tissue in the turbinates. It is a precise method that helps in reducing the size of the turbinates. Laser turbinate reduction is performed under local or general anesthesia.
Submucosal Turbinate Reduction – This surgical technique involves removing or reducing the size of the turbinates from within the mucosal layer. It aims to maintain the outer structure of the turbinates while addressing the underlying cause of obstruction.
Coblation Turbinate Reduction – Coblation utilizes low-temperature radiofrequency energy in a saline solution to remove or reduce turbinate tissue. It is a gentle approach that minimizes damage to surrounding tissues.
Microdebrider Turbinate Reduction – A microdebrider, a powered cutting device, is used to trim and remove excess turbinate tissue. This method allows for precise tissue removal with minimal bleeding.
Traditional Turbinate Reduction Surgery – In more severe cases, traditional surgical methods may be employed. This can involve partial or complete removal of the turbinate tissue to alleviate nasal obstruction.
The choice of turbinate reduction surgery depends on the individual’s specific condition, the severity of symptoms, and the surgeon’s expertise. It is essential for individuals considering these procedures to consult with an Ear, Nose, and Throat (ENT) specialist who can assess their condition and recommend the most suitable approach.
Turbinate Reduction Surgery Insurance Coverage
Turbinate reduction surgery, also known as turbinate coblation or turbinoplasty, involves reducing the size of nasal turbinates to alleviate symptoms like chronic nasal congestion. The procedure is performed using various techniques, including radiofrequency ablation, laser surgery, or traditional surgical methods.
Medical Necessity: Insurance coverage for turbinate reduction surgery is often contingent on the medical necessity of the procedure. If the surgery is deemed necessary to address a specific medical condition, insurance is more likely to cover it. Conditions such as chronic nasal obstruction, sleep apnea, or recurrent sinus infections may be considered valid reasons for medical necessity.
Pre-authorization: Many insurance providers require pre-authorization before approving coverage for turbinate reduction surgery. This involves obtaining approval from the insurance company before the surgery takes place. A thorough evaluation by a healthcare professional, including documentation of symptoms and failed attempts at non-surgical treatments, may be necessary for pre-authorization.
In-Network Providers: Insurance plans typically have a network of preferred healthcare providers. Using an in-network provider for turbinate reduction surgery increases the likelihood of insurance coverage. Before scheduling the surgery, it’s advisable to confirm that both the surgeon and the facility are within the insurance network.
Policy Specifics: Insurance coverage can vary significantly based on the specific policy and plan chosen by the individual. Some policies may explicitly exclude coverage for certain procedures, while others may cover turbinate reduction surgery under certain conditions. Reviewing the policy details and contacting the insurance provider for clarification is crucial.
Tips for Navigating Insurance Coverage

Obtain Pre-Authorization: In many cases, pre-authorization is a key step in securing insurance coverage for turbinate reduction surgery. Work closely with the healthcare provider’s office to submit all required documentation and obtain the necessary approvals from the insurance company.
Verify In-Network Providers: To maximize insurance coverage, verify that both the surgeon and the surgical facility are within the insurance network. Out-of-network providers may result in higher out-of-pocket costs for the individual.
Document Failed Conservative Treatments: Insurance providers often require documentation of failed attempts at conservative treatments before approving surgery. Get a copy of your medical records, especially all non-surgical interventions such as medications, nasal sprays, or allergy treatments that were not effective in alleviating your symptoms.
Appeal Process: If the initial request for coverage is denied, individuals have the right to appeal the decision. The appeal process allows for additional documentation or clarification to support the case for medical necessity. Engage with your turbinate reduction surgeon’s office to navigate the appeals process.
Key Takeaways
In conclusion, insurance coverage of turbinate reduction surgery is contingent on several factors, including medical necessity, pre-authorization, in-network providers, and policy specifics. Individuals considering this surgery should proactively engage with healthcare professionals, thoroughly understand their insurance policies, and follow the necessary steps to increase the likelihood of coverage. While the process may involve some administrative hurdles, the potential benefits of improved nasal function and quality of life make it a journey worth undertaking for many individuals.
Always consult with healthcare providers and insurance representatives for personalized guidance based on individual circumstances.